A Message from Our Program Director
The Internal Medicine Residency Program of Westchester Medical Center/New York Medical College is committed to providing outstanding training in Internal Medicine.
We motivate each house officer to embrace a critical and probing scientific attitude, along with a commitment to reducing health disparities. As a tertiary referral center, Westchester Medical Center is among the highest case mix index in the region. The Cardiology, Transplant, and Critical Care services care for patients from throughout the Hudson Valley. Our diverse patient population provides a robust clinical and educational experience for training physicians. House staff interacts with full-time faculty members from all divisions regularly for mentorship, didactics and clinical supervision. All mandatory training, including resident continuity clinic, is provided on site.
The university hospital shares a large picturesque campus with New York Medical College, including the schools of medicine, dentistry, graduate school of basic medical sciences, and school of health sciences. This close proximity provides integration of medical student education as well as numerous teaching and precepting opportunities for the house staff. The medical school has a new translational research center that provides the infrastructure to conduct high quality research by utilizing the resources offered by New York Medical College and clinical investigators at Westchester Medical Center.
Recent enhancements to the program include the creation of a Director of Research for the Division of Internal Medicine. The position is held by Dr. Christopher Nabors, who has received national recognition for his quality and safety projects, which have led to many scholarly projects for the department. New educational venues include telemedicine, a formal point-of-care ultrasound training program, and increased use of the simulation center. Hospital-wide initiatives to advance safety and quality improvement include the expansion of a telehealth unit and increased collaboration with the quality improvement department.
Fellowships are available in all approved areas of subspecialty training at the Medical Center, and WMC house staff are highly successful at obtaining fellowships of their choice at the medical center and throughout the country.
Please be sure to take a look at the fellowship placement of our program graduates on the "Graduate Fellowship Placement" tab.
The Internal Medicine Residency Training Program at Westchester Medical Center follows our institutional commitment to foster diverse and inclusive environments that support personal and professional growth. We adhere to the AAMC best practices for recruitment with an emphasis on diversity and inclusion, and we welcome applications from all backgrounds. Our recruitment process ensures that all underrepresented groups are given equal opportunities. Our program directly collaborates with the Chancellor of Diversity at New York Medical College in our ongoing efforts to provide an inclusive environment for our trainees throughout the course of residency. Westchester Medical Center provides many development and wellness opportunities including a variety of diversity and inclusion topics for our faculty and trainees.
Program Overview and Curriculum
Program Structure
The Internal Medicine Residency Program at Westchester Medical Center has 63 categorical residents. Through collaboration with the WMC Anesthesiology and Neurology residency programs, 20 additional categorical base year interns train with our program during their first year. In July of 2024, we will have four additional interns as part of the new Physical Medicine and Rehabilitation Residency at WMC. All core rotations are located on the Valhalla campus.
Our program follows a 6 + 2 schedule (six weeks inpatient; two weeks ambulatory). Below is an example of our current annual schedule.
PGY1
- 10-14 weeks: Medicine floors
- Four to six weeks: Specialty floors (Transplant and General Cardiology Service)
- Four to six weeks: Medical Intensive Care Unit (MICU)
- Two to four weeks: Cardiac Care Unit (CCU)
- Six to eight weeks: Elective
- Four to six weeks: Night Float
- Eight to 10 weeks: Ambulatory Clinic
- Two to four weeks: Medicine Consults / Admitting team
- Four weeks: Vacation
PGY2
- Four to eight weeks: General floors
- Four to eight weeks: Specialty floors (Transplant or General Cardiology Service)
- Eight to 10 weeks: Elective (including 2-week Neurology selective)
- Two to four weeks: MICU
- Two to four weeks: CCU
- Six to eight weeks: Night Float / CCU Night Float / ICU Night Float
- One to two weeks: Night Float cross coverage (5 nights/week)
- Eight to 10 weeks: Ambulatory Clinic
- Two to four weeks: Medicine Consults / Admitting team
- Two to four weeks: backup home call
- Four weeks: Vacation
PGY3
- Six to eight weeks: General floors
- Two to four weeks: Oncology (Solid Tumor) inpatient service
- Eight to 10 weeks: Electiv
- Two to four weeks: MICU
- Four to six weeks: Night Float / ICU Night Float
- Eight to 10 weeks: Ambulatory Clinic
- Two to four weeks: ICU Consults
- Four to six weeks: Medicine Consults/Admitting team
- Two to four weeks: backup home call
- Four weeks: Vacation
A Typical Day on the Floors
7 a.m. Morning Sign-in
7:30 a.m. Morning Report (on Tuesday and Thursday)
9 a.m. Hospitalist Team Bedside Rounds
12 - 4 p.m. Varied Didactic Series
5 p.m. Sign-Out
Floor Call
On weekdays every fourth night from 5 p.m. – 9 p.m.
Floor Night Float
Senior Residents: Six nights/week from 9 p.m. – 7 a.m. (Monday – Sunday)
PGY1 Residents: Two to three nights off per two-week block
Ancillary Services
- 24/7 phlebotomy shifts
- IVs & PICC/midlines by trained nurses
- EKG technicians 24/7
- Patient transport support
- Patient experience representation seven days/week
Conference & Didactics
The didactic are scheduled in topic blocks and provided by subspecialists to facilitate structured approach to reading and board preparation. Primary focus of the curriculum is to prepare residents for ABIM boards and to equip them to be mature and confident clinicians. Didactics comprises of subject blocks throughout the academic year, covering all core subjects for board preparation. This also includes weekly board review sessions run by the Chief Resident.
All lectures are presented in person and virtually. They are also recorded and archived for future viewing opportunities. Residents also have protected didactic experiences one half-day per week during each ambulatory rotation.
Subscription to MKSAPS provided by institution for PGY2 and PGY3 residents.
Grand Rounds
On Wednesdays, we have departmental grand rounds from 12 – 1 p.m. for all PGY levels where distinguished guests present topics of interest and engage with the house staff and faculty in scholastic discussions.
Morning Report
Morning report takes place every Tuesday and Thursday at 7:30 a.m. for PGY2 and PGY3 residents to discuss overnight admissions and recent interesting cases.
Chair Rounds
Weekly chairperson rounds take place every Friday from 12 – 12:45 p.m. where an on-call intern presents an interesting case from the floors, moderated by senior faculty.
Senior Specialty Sessions
Every Friday from 1 - 1:45 p.m., there is a rotation of CCU, MICU, M&M and Research Forums for PGY2 and PGY3 residents.
Monthly Journal Club
Once per month on Monday afternoon, led by senior faculty and all levels are encouraged to participate.
Medicine Departmental Conferences
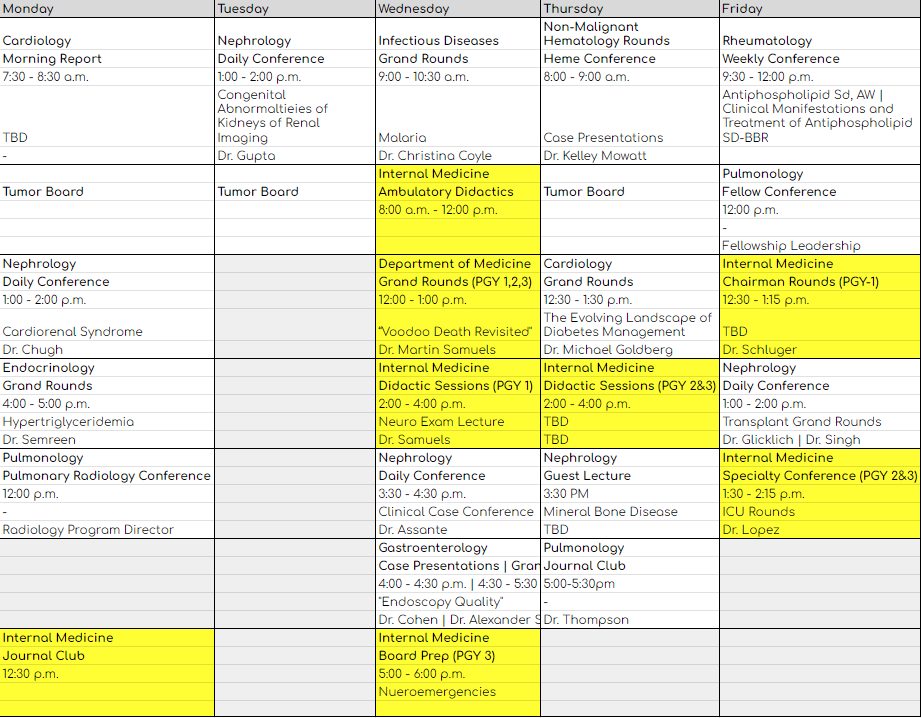
Because Westchester Medical Center has a comprehensive array of residency and fellowship programs, each day there is a wide variety of educational conferences. Below is an example of a one-week period of Department of Medicine conferences. There are numerous conferences every day in the departments of Neurology, Surgery, Radiology and Anesthesia among others that all are open to all. There are also several conferences broadcast weekly from New York Medical College.
Clinical Skills Education
Our educational simulation experiences include utilization of simulation venues at both Westchester Medical Center (the Point of Care Simulator and Surgical Skills Lab) and New York Medical College (simulation center with multiple simulators and patient actors). We collaborate with advanced nursing educators and multiple other specialty services to advance communication, procedural and practical skills in a variety of settings.
Graduate Fellowship Placement


Fellowship Matches 2016 - 2021
Allergy and Immunology
Rutgers-New Jersey Medical School
Cardiology-Cardiovascular Disease
Brown University
Mount Sinai Beth Israel
Montefiore/Albert Einstein Hospital
University of Miami Health System
Maimonides Hospital
Methodist Hospital
Lehigh Valley Health Network
Loma Linda University
Montefiore Hospital
Newark Beth Israel Medical Center
Tulane University
Tulane University
University of Oklahoma
University of Texas at Houston
Westchester Medical Center x5
Cardiology-Interventional
Columbia University
Cardiology-Research
Kansas Medical Center
Cardiology-Structural Interventions
Houston Methodist Hospital
Clinical Nutrition
Cleveland Clinic
Endocrinology, Diabetes and Metabolism
Einstein College of Medicine / Montefiore Medical Center
Dartmouth Hitchcock Medical Center
University of Alabama at Birmingham
Gastroenterology
Henry Ford Health
Oakland University William Beaumont
University of Connecticut x2
University of Iowa
Westchester Medical Center x5
Gastroenterology-Advanced Endoscopy
Stony Brook University Hospital
Heal Initiative
University of California-SF
Hematology & Medical Oncology
Baylor College of Medicine
North Shore University / Long Island Jewish Medical Center
SUNY Downstate Medical Center
University of Vermont
Westchester Medical Center x3
Infectious Diseases
Northwell Health
Westchester Medical Center
Medical Education
Boston University
Nephrology
Baylor College of Medicine
Beth Israel Deaconess Hospital
Icahn School of Medicine @ Mount Sinai
Massachusetts General Hospital
New York University
University of Washington-Seattle
Westchester Medical Center x4
Pulmonary & Critical Care Medicine
Albany Medical College
Mayo Clinic-AZ
New York Presbyterian Hospital-Queens
Spectrum Health @ Michigan State University
Saint Louis University
Westchester Medical Center x4
Rheumatology
Loma Linda University
University of Connecticut
University of Southern California
Washington University in St. Louis
Westchester Medical Center x3
Program Leadership

Edward Lebovics, MD
Interim Director, Department of Medicine
Edward Lebovics, MD, is the Sarah C. Upham Professor of Gastroenterology. Dr. Lebovics has been the Director of the Division of Gastroenterology and Hepatobiliary Diseases since 1997. He currently serves as President of the Medical Executive Committee at WMC and on the Executive Committee of the Faculty Senate at NYMC. He has directed the Gastroenterology Fellowship Program from 1997 to 2017. His achievements have been recognized by a Certificate of Special Congressional Recognition and by election to Fellowship at the American College of Physicians, American College of Gastroenterology, American Gastroenterological Association and American Association for the Study of Liver Diseases. He has been regularly listed amongst "Top Doctors" by New York Magazine and various other publications. Dr. Lebovics has authored numerous articles and book chapters and delivered many invited lectures. Medical students and residents have recognized his commitment to teaching through Excellence in Teaching Awards.
Professional Interests: advanced therapeutic endoscopy, biliary and pancreatic endoscopy, hepatitis B and C virus infection, non-alcoholic fatty liver disease, chronic cholestatic diseases, and inflammatory bowel disease.

Leanne Forman, MD
Program Director
Dr. Forman was appointed program director in 2017 after serving in leadership positions in the residency as the Section Chief and Director of Outpatient Medicine for more than ten years. Dr. Forman has more than 25 years of experience in graduate and undergraduate medical education at several distinguished institutions. She has consistently been recognized for excellence in teaching and contributions to the program. The program continuously strives to anticipate the needs of the physicians of today and tomorrow. The educational process focuses on the acquisition of medical knowledge, utilization of evidence, and development of clinical skills, as well as emerging practice patterns.

Jason Goutis, MD
Associate Program Director
Interim Director, Adult Ambulatory Care Clinic
After majoring in Biochemistry at Tufts University and obtaining a master’s degree in Physiology from Georgetown University, Dr. Goutis attended medical school at the Universidad Autónoma de Guadalajara in Mexico. He completed a required fifth year through New York Medical College, after which he completed his residency in internal medicine at Westchester Medical Center. After residency, Dr. Goutis joined the faculty at WMC and currently is involved in supervising and teaching residents primarily in the outpatient continuity clinic. He is the Director of the Point-of-Care Ultrasound Program for internal medicine, as well as the Chair of the Quality Assurance Process Improvement Committee. He also has special interest in global medicine and medical missions.

Ramachandra Reddy, MD
Associate Program Director
Dr. Ramachandra Reddy graduated from Albert Einstein College of Medicine in 2016 and completed his Internal Medicine residency at Mt. Sinai Hospital where he was named Educator of the Year due to his excellence in medical student and resident education. He then completed a fellowship in Hematology and Oncology at New York University where he was named as Fellow of the Year twice for his outstanding clinical skills. He has been nominated to the Gold Humanism Honor Society for his compassionate patient care.
Throughout his training Dr. Reddy has demonstrated expertise in medical education by providing lectures, serving as a tutor for step exams and developing curricula at both student and resident levels including one that was presented at a national conference. He is passionate about medical education and in his new role as an Associate Program Director for the Internal Medicine Residency he will serve as a strong liaison and educational coordinator for both the Hematology/Oncology fellows and medicine house staff.

Latif Salam, MD
Associate Program Director
Dr. Latif Salam holds a position of Attending Physician and Clinical Assistant Professor of Medicine. Before coming to Westchester Medical Center, Dr. Salam served as teaching faculty at SUNY Downstate Health Sciences University in Brooklyn, NY where he spent the last seven years as an Academic Hospitalist in the Department of Medicine. He was a member of the SUNY Downstate College of Medicine Admissions & Interview Committee. He has received multiple prestigious awards including Teacher of the Year in recognition of his dedication to teaching and academic medicine. Dr. Salam completed his Internal Medicine Residency Training at New York Presbyterian-Brooklyn Methodist Hospital/Weill Cornell Medical College. He is board certified in Internal Medicine and a fellow of the American College of Physicians. Dr. Salam holds strong interest in healthcare disparity amongst minorities and in mentorship of medical students interested in Internal Medicine specialty.

Liana Tatarian, DO
Associate Program Director
Dr. Tatarian is Associate Residency Program Director and Assistant Professor of Medicine at New York Medical College. She completed her Internal Medicine Residency through the Stony Brook University Hospital system where she was appointed Chief Resident for her exceptional leadership skills. Following completion of residency, she joined Westchester Medical Center in 2021 as an Academic Hospitalist. She is deeply passionate about resident education and looks forward to mentoring the next generation of exceptional physicians.

Andrea Porrovecchio, MD, FACP
Section Chief, Division of General Internal Medicine, Westchester Medical Center
Clinical Assistant Professor of Medicine, New York Medical College
Dr. Porrovecchio completed her medical degree from New York Medical College in June 2002. She completed her Internal Medicine Residency at Keesler Medical Center in June 2005 while serving on active duty in the United States Air Force. She was recruited to join the faculty at the Montefiore/Einstein in the Division of Hospital Medicine as an academic hospitalist after completing her active duty commitment to the USAF in 2008. She held multiple leadership roles there including Director of the Medical Service and the Associate Program Director of the Internal Medicine Residency at the Wakefield Campus. She came to Westchester Medical Center as the Section Chief for General Internal Medicine in September 2020. Her interests include Quality and Process Improvement and Point of Care Ultrasound.
Educational Program Liaisons
Neurology

Liana Tatarian, DO
Associate Program Director
Dr. Tatarian is Associate Residency Program Director and Assistant Professor of Medicine at New York Medical College. She completed her Internal Medicine Residency through the Stony Brook University Hospital system where she was appointed Chief Resident for her exceptional leadership skills. Following completion of residency, she joined Westchester Medical Center in 2021 as an Academic Hospitalist. She is deeply passionate about resident education and looks forward to mentoring the next generation of exceptional physicians.
Anesthesiology

Neal Shah, MD
Dr. Shah is an Assistant Professor of Internal Medicine, part of the teaching faculty here at Westchester. He completed his residency at Drexel University followed by serving as faculty at Temple University. Dr. Shah also serves as the Internal Medicine liaison for the categorical anesthesia residents.
General Medicine Faculty
Hospitalists
Andrea Porrovecchio, MD, FACP
Section Chief, Division of General Internal Medicine, Westchester Medical Center Clinical Assistant Professor of Medicine, New York Medical College
Ronald Cho, MD
Clinical Assistant Professor of Medicine, New York Medical College
Aditi Desai, MD
Leanne Forman, MD
Clinical Associate Professor of Medicine, New York Medical College
Richard Gil, MD
Clinical Assistant Professor of Medicine, New York Medical College
Randy Goldberg, MD, MPH, FACP
Assistant Professor of Medicine, New York Medical College
Jason Goutis, MD
Instructor of Medicine, New York Medical College
Gary Guo, MD, PhD
Instructor of Medicine, New York Medical College
Shalini Harigovind, MD
Clinical Assistant Professor of Medicine
Alexander Hrycko, MD
Clinical Assistant Professor of Medicine
Faisal Jamal, MD
Clinical Assistant Professor of Medicine, New York Medical College
Chikere Kanu, MD
David Kastrinsky, MD
Mariana Kawalet, MD
Sora Lee, MD
Stephen Lobo, MD, FACP
Associate Hospital Epidemiologist, Department of Infection Prevention and Control, Westchester Medical Center Clinical Assistant Professor of Medicine, New York Medical College
Kelsey McManus, MD
Arif Mumtaz, MD
Associate Professor of Medicine, New York Medical College
Christopher Nabors, MD, PhD
Assistant Professor of Medicine, New York Medical College
Jacob Ouseph, MD
Clinical Assistant Professor of Medicine, New York Medical College
Vincent Prawoko, MD
Hasan Rahmatullah, MD
Clinical Assistant Professor of Medicine, New York Medical College
Ramachandra Reddy, MD
Mitra Rezvani, MD
Clinical Assistant Professor of Medicine, New York Medical College
Shushunova Sangia, MD
Latif Salam, MD
Clinical Assistant Professor of Medicine
Neal Shah, MD
Clinical Assistant Professor of Medicine, New York Medical College
Merita Shehu, MD
Assistant Professor of Medicine, New York Medical College
Tejinderpal Singh, MD
Assistant Professor of Medicine, New York Medical College
Liana Tatarian, DO
Clinical Assistant Professor of Medicine, New York Medical College
Eric Wold, MD
Assistant Professor of Medicine, New York Medical College
Outpatient Medicine Faculty
Shick Yu, MD
Assistant Professor of Medicine, New York Medical College
Resident Continuity Clinic Preceptors
Christine Carosella, MD, FACP
Clinical Assistant Professor of Medicine, New York Medical College
Leanne Forman, MD
Clinical Associate Professor of Medicine, New York Medical College
Melissa Gennarelli, MD
Clinical Assistant Professor of Medicine, New York Medical College
Rebecca Glassman, MD
Assistant Professor of Medicine, New York Medical College
Jason Goutis, MD
Instructor of Medicine, New York Medical College
Christopher Nabors, MD, PhD
Assistant Professor of Medicine, New York Medical College
Brooke Nevins, MD
Student Education Faculty
Melissa Gennarelli, MD
Site Director, Third Year Internal Medicine Clerkship, New York Medical College
Clinical Assistant Professor of Medicine, New York Medical College
Kausik Kar, MD
Internal Medicine Sub-Internship Director, New York Medical College
Assistant Professor of Medicine, New York Medical College
Mitra Rezvani, MD
Internal Medicine Clerkship Director, New York Medical College
Clinical Assistant Professor of Medicine, New York Medical College
Tejinderpal Singh, MD
Assistant Site Director for Third-Year Clerkship
Assistant Professor of Medicine, New York Medical College
Gary
KKar, MD
Internal Medicine Sub-internship Director, New York Medical College
Assistant Professor of Medicine, New York Medical Co
Gary Stallings, MD, MPH
Associate Chair for Undergraduate Clinical Education
Assistant Dean for Clinical Sciences, New York Medical College
COVID-19 Vaccination Requirements
Please note: our program follows institutional, state and federal COVID-19 vaccination requirements for healthcare workers. We encourage you to monitor these requirements frequently as they are subject to change. Please contact our program coordinator if you have any questions.
Program Signaling
While we preferentially review applications from those who signal our program, we also consider applicants who do not signal us.
FAQ
What schedule structure does the program utilize?
The program follows a 6+2 schedule. Residents rotate through General Medicine Floors, ICU, electives, and clinic.
What kind of opportunities are there for residents interested in subspecialties?
WMC has nearly every subspecialty of medicine available in house. Internal Medicine residents rotate through multiple subspecialties, such as Liver Transplant and General Cardiology Service for core rotations. Additionally, residents have the opportunity to experience subspecialties through elective blocks.
How are research projects initiated?
Every resident meets with the Director of Research in the beginning of the year to establish research mentors and research projects.
How does the resident call schedule work?
Residents are on call every 3rd or 4th day while on General Medicine Floors and ICU.
How does the program structure elective time?
Electives are interspersed throughout the schedule. All residents participate in core electives including Infectious Diseases, Endocrinology, Nephrology, Hematology, Rheumatology, and Oncology. In addition to these core electives, residents have the freedom to pursue any specialty that interests them.
Are there good opportunities for performing procedures?
Residents have many opportunities to perform ABIM required procedures as well as a variety of elective procedures. These include but are not limited to Central Line Placement (Internal Jugular, Femoral, and Subclavian), Pap Smears, Lumbar Puncture, and Ultrasound guided IV placement.
How does the program conduct didactics?
Our program includes a wide variety of didactics to maximize resident educational experience. These include but are not limited to Noon Conferences, Morning Reports, ICU Rounds, CCU Rounds, Kidney Rounds, Chairman Rounds, Clinical Reasoning Sessions, Morbidity and Mortality Meetings, Journal Clubs.
What do residents do outside of work?
Westchester County has a wide variety of exciting activities. Whether you are interested in hiking, restaurant hopping or live music, you can always find something fun to do here. We are also located just 40 minutes north of New York City, so it’s just a quick drive or train ride away.
What housing accommodation options are available?
There are many apartments and other housing units available for rent throughout Westchester and surrounding areas. Many residents live in the City of White Plains, which is about a 15-minute drive from campus. Other popular areas include Tarrytown, Sleepy Hollow, Yonkers, and Peekskill. A limited amount of on-campus housing is available to interns for their first year of training only.
Does the program accommodate requests for Maternity leave?
Our program adheres to ACGME and ABMS guidelines for leave requests.
Does the program provide board-review preparation resources?
All PGY-2 and PGY-3 residents in our program are provided with full membership to NEJM Resident 360 and Knowledge+.
Is there financial support for educational activities?
Residents have access to an educational allowance through the CIR Continuing Learning Program. Resident first authors on research projects are fully supported for regional and national meeting attendance and presentation.
How are residents evaluated?
Residents are evaluated by attendings and/or fellows on every rotation. The evaluation results are shared with the residents at the time they are completed, and the resident is asked to acknowledge and sign off on each.
How can residents provide feedback to program leadership?
An anonymous electronic survey is open continuously, in which residents are encouraged to share ideas, questions and concerns. The results of this survey are shared with program leadership and acted on accordingly.
Is the program receptive to feedback?
Our program takes the concerns of our residents incredibly seriously. Our trainees are encouraged to reach out to program and departmental/institutional leadership immediately if they feel there is an issue that needs to be addressed. Residents are requested to anonymously evaluate each rotation they complete, and this feedback is analyzed by program leadership and utilized to develop action plans.
How to Apply
The following are general guidelines for applying to the program. The information provided should answer most of your questions.
Thank you for your interest in the Westchester Medical Center/New York Medical College Internal Medicine Residency Training Program at Westchester Medical Center. Together, they comprise a major academic medical center. Our program is fully accredited by the Accreditation Council for Graduate Medical Education (ACGME).
Criteria for Applicants
Applications should be submitted through the Electronic Residency Application System (ERAS), which can be accessed using the following link: https://apps.aamc.org/myeras. Applications may be submitted starting September 6, 2023.
Internal medicine residency programs may begin reviewing applications in ERAS on September 27, 2023. We will notify applicants through ERAS as to whether they have been selected for an interview.
In accordance with recommendations from the Association of American Medical Colleges and the Alliance for Academic Internal Medicine, our residency interviews for the 2023-2024 application cycle will be held virtually.
Our program will begin our first round of invitations in early October. Applications will not be reviewed after October 20, 2023. Interviews will take place from October through January, and candidates will be provided with detailed information regarding the logistics of the interview days.
USMLE or COMLEX Steps 1 and 2 must be passed in order to be considered (step 2 results can be pending at the time of interview but must have a passing score in order to be ranked).
Applicants need at least three letters of recommendation dated within the current academic year. There is no particular requirement for which type of faculty/supervisors write your letters. We prefer that they are written by faculty who are the most familiar with applicants.
Please note:
- We do not have a firm cut off on USMLE or other exam scores. We review all applicants from a holistic standpoint, considering their overall diversity, skills, and experience.
- While we prefer candidates not more than five years out of medical school, an applicant involved in a post-graduate clinical environment will be considered.
Visa Sponsorship
Passage of USMLE Step 3 is strongly encouraged for all applicants applying from abroad.
Westchester Medical Center will sponsor J-1 visas. If needed, applicants can obtain Exchange Visitor Sponsorship through the Educational Commission for Foreign Medical Graduates (ECFMG) to acquire a J-1 visa.
H-1B visas may be considered on a case by case basis for the most highly qualified candidates. If seeking H-1B sponsorship, you must inform the program directly at the time you apply through ERAS. If granted H-1B consideration from the program, in order to be ranked, it is mandatory for you to have taken and passed Step 3 of the USMLE prior to the rank order list deadline.
More information about the residency program is available on our Fellowship and Residency Electronic Interactive Database (FREIDA) listing.
Contact Us
Austin Charnis
Residency Program Manager, Internal Medicine
Austin.Charnis@WMCHealth.org
Austin Charnis, a native of Westchester County, has been the administrator of the Internal Medicine Residency Program at Westchester Medical Center since 2019. Prior to this role Austin held positions at our institution as fellowship coordinator in medicine subspecialties and administrative assistant in the Office of Graduate Medical Education. His professional interests include medical education, communications and technology, and he is highly passionate about supporting our residents, faculty and staff.