Welcome to MFCH Pediatric Critical Care
Thank you for choosing to explore the Pediatric Critical Care Medicine Fellowship Program at Maria Fareri Children’s Hospital (MFCH) at Westchester Medical Center (WMC). We hope that the information on this site is helpful and that you will consider our program in your application process.
The Pediatric Critical Care Medicine Fellowship is a three-year ACGME-accredited training program fit for physicians passionate about providing the best clinical care and supporting patients, families, and caregivers throughout the process. Our mission is to train excellent pediatric intensivists in all aspects of pediatric critical care by providing both the knowledge and skills required to provide top-quality, evidence-based medicine to our patients in a family-centric environment.
Our fellows will become experts in the physiology and management of both common and rare diseases, their treatments, and common procedures required to ensure delivery of outstanding clinical care. In addition, we will foster independent learning and communication skills with all members of the team, including colleague physicians, trainees, other caregivers, and parents.
Maria Fareri Children’s Hospital at Westchester Medical Center resides in a high-volume, high-acuity, tertiary care facility and serves the tri-state area and beyond. We are proud to feature the only Level 1 Pediatric Trauma Center and Pediatric Burn Center in the Hudson Valley, in addition to all pediatric medical and surgical subspecialties, which allow us to support the needs of all children in the communities that we serve.

Erin Rescoe, MD
Program Director, Pediatric Critical Care Medicine Fellowship
Attending Physician, Pediatric Critical Care Medicine, Maria Fareri Children’s Hospital at Westchester Medical Center
Assistant Professor, Pediatrics, New York Medical College
Overview
Our Pediatric Critical Care Medicine fellows’ primary learning environment provides access to active medical and surgical subspecialty services, including the Hudson Valley's only Level 1 Trauma Center, as well as an active pediatric cardiothoracic surgery service which provides our fellows a diverse education in post-operative management. In addition, the fellow will have an augmented pediatric CVICU experience in a dedicated Cardiac Unit at Mount Sinai Kravis Children's Hospital for a deeper experience in cardiac critical care. Fellows here will earn graduated autonomy according to their unique skills and will be supported twenty-four hours a day by in-house PCCM attendings.
Our PICU is an 18-bed mixed medical and surgical unit and provides care for the sickest and most acute patients. We utilize all advanced modes of ventilation including HFOV. We are a pediatric ECMO center that provides both veno-venous and veno-arterial ECMO for medical and surgical patients. We also support all modes of dialysis including CRRT.
Our fellows will work closely with our strong subspecialty teams, complemented by interaction with other fellowship programs in Pediatric Hematology/Oncology, Pediatric Pulmonary, Pediatric Gastroenterology and Pediatric Hospital Medicine, which provide learning and research opportunities in a wide range of subjects. In addition, the PCCM faculty are actively engaged in teaching and mentoring residents and are looking forward to helping develop the next generation of PCCM physicians.
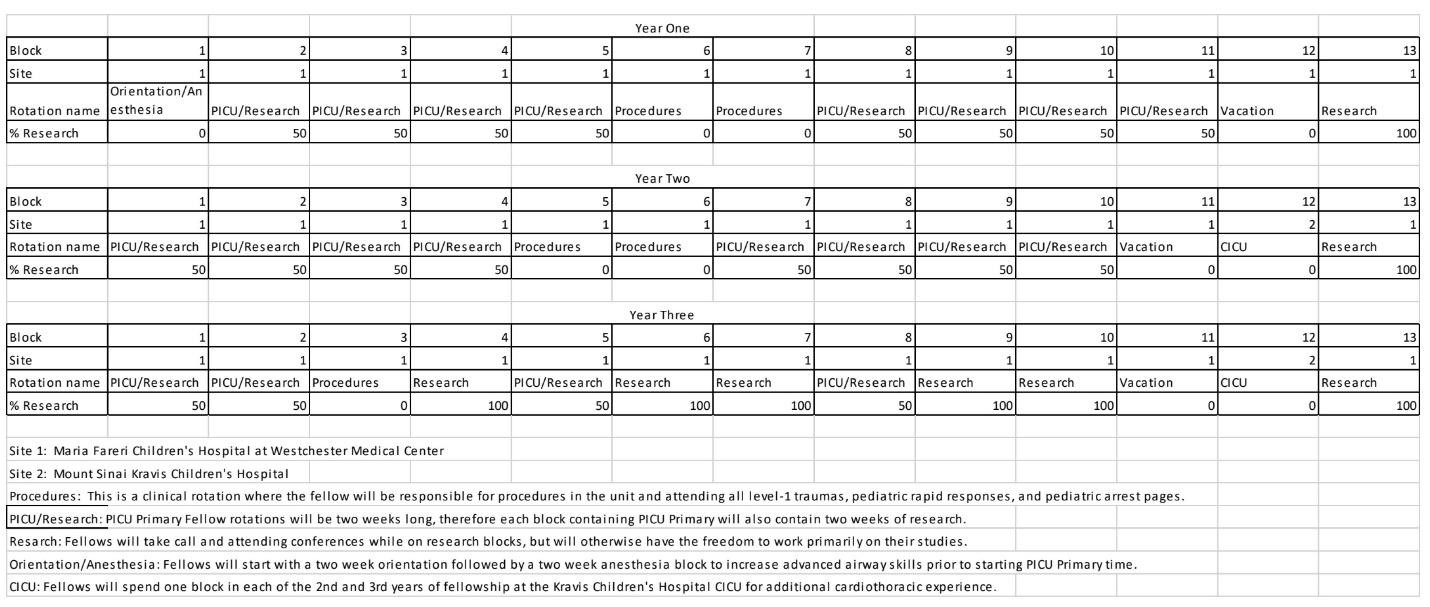
The Pediatric Critical Care Medicine Fellowship Program wills include three to four months of service time each year. In years two and three of fellowship, trainees will get additional experience in the CVICU at Kravis Children’s Hospital. Fellows will also take in-house calls covering the PICU at Maria Fareri Children’s Hospital.
Curriculum
The fellow will be expected to run the pediatric critical care service at MFCH during their assignments to the PICU, which includes rounds, admissions, and bed-management as well as being the primary physician for families or caregivers. Fellows will also be expected to teach residents and medical students during this time.
CICU blocks are specific to years two and three where the fellow will run the CVICU service at Mount Sinai Kravis Children’s Hospital.
During their educational experiences devoted to performing and developing competence in procedures, fellows will be in-house during the day in a backup and consult role. The fellow will be first call for all procedures required in the unit throughout the day, either assisted or solo depending on the fellow’s individual skill level, as well as consults in the emergency department, pediatric general medicine floor, and pediatric recovery room. During this time, the fellow will also carry the code pager and be expected to respond to all arrests, rapid responses, and Level-1 Traumas.
Research blocks will be independent time for the fellow to pursue their scholarly project. Fellows will be supported by a faculty mentor while they explore their potential research interests with the goal of identifying a research mentor and project in the first year of fellowship. This may be basic, translational, clinical, or education related. The fellow will have access to all MFCH faculty as well as the New York Medical College research infrastructure to assist them. During their research blocks they will still be required to attend all conferences during this time and have on-call responsibilities.
Below is a generic example of a rotation schedule assignment.