A Message from Program Director
Thank you for your interest in the Pediatric Residency Program at Westchester Medical Center at the Maria Fareri Children's Hospital (MFCH), a member of the Westchester Medical Center Health Network (WMCHealth). We hope the information located here will further your interest in our program by conveying its many strengths
Our program's mission is to produce outstanding pediatricians who are ready to excel in both general and subspecialty pediatrics. To achieve this, we create an educationally innovative, inclusive and supportive environment and foster camaraderie and teamwork amongst our physicians. Our residents receive an exceptional education in all areas of pediatrics and they acquire the practical skills needed to care for children with a vast range of illnesses.
Our location in New York's Hudson Valley grants us unparalleled population density and diversity. MFCH is the principal referral center of the Hudson Valley, the 150-mile region between New York City and Albany; this ensures that our residents manage childhood illnesses that range from common, to rare, to previously undescribed. Year after year our residents express enthusiasm about the diversity of our cases and the educational opportunities provided by the breadth of pathologies we encounter. Our administrative leadership and extensive teaching faculty strive to maximize the educational opportunities offered by our diverse patient population. We pride ourselves on our program’s supportive, inclusive culture that values advocacy and joy in our work.
MFCH provides a state-of-the-art environment for our clinical, educational, and research activities. MFCH is a full-service children's hospital with complete pediatric subspecialty representation. Designed with the comfort of both families and caregivers in mind, MFCH features on-call suites for our residents and numerous conference areas.
The first children's hospital named after a child, MFCH has set the standard for a comforting and stimulating healing environment for ill children and their families. We offer private rooms for every patient with sleeping space for parents, family housing at our on-site Ronald McDonald house, a giant aquarium, an interactive computer lab/music studio, the world's largest dollhouse, a baseball museum, and a wheelchair-accessible miniature golf course.
Our program is fully accredited by the Accreditation Council for Graduate Medical Education. We strictly observe both New York State and Residency Review Committee regulations regarding resident work hours and supervision.
We are proud of our program and its graduates, and we look forward to introducing them to you.
Sincerely,
Matthew J. Kapklein, MD, MPH
Program Director
Caroline Moon, MD, MTS
Associate Program Director
Sonia Solomon, DO
Assistant Program Director
Program Overview
Didactic Education
Our program is committed to resident education with protected educational time for daily clinical reason conference, noontime core conference and weekly resident-led continuity clinic conference.
Our pediatric residency program Zoom ID is 477.318.5601. Feel free to pop in just about every Monday, Tuesday, Thursday and Friday from 8 -9 a.m. (clinical reasoning conference) and every weekday 12 p.m. - 1 p.m. (noontime core conference) to get a glimpse of our daily education and resident life!
Clinical Reasoning Conference (CRC)
During clinical reasoning conference, select overnight admissions are presented by residents to their peers and selected faculty. Emphasis is placed on clinical diagnostic reasoning and decision making as we work through initial patient presentations while discussing differential diagnoses.
Noontime Core Conference
Noontime core conference consists of a boards-based curriculum that is supplemented by a variety of educational topics in all pediatric subspecialty areas as well as wellness sessions, journal club, resident-as-teacher presentations, pediatric board review sessions, emergency medicine skills workshops, critical care lectures and monthly house staff meetings.
Continuity Clinic Conference
Every week during continuity clinic sessions, residents discuss topics from our online curriculum, which covers a wide range of topics relevant to primary pediatric care, including; nutrition, developmental milestones, vaccine schedules, breastfeeding versus formula feeding, and anticipatory guidance.
Grand Rounds
Grand rounds occur every Wednesday from 8:00 - 9:00 and are open to all faculty, residents, and medical students. Here, faculty and residents, as well as guest lecturers, present a variety of pertinent pediatric topics.
Board Review
In addition to our daily morning clinical reasoning conference and noontime core conference, residents are given an annual subscription to the TrueLearn Question Bank, our online curriculum for the weekly lectures in continuity clinic, the Challenger Question Bank, and PREP Question Banks through FREE AAP memberships. During the spring of third year, senior residents participate in a board review boot camp in preparation for their upcoming boards.
Simulations
We have regularly scheduled mock codes and monthly PICU simulations. Simulated resuscitations are also frequently held in our NICU. Additionally, we hold PICU boot camps, IV placements, splinting and suture workshops that are frequently provided throughout the year for our residents. We participate in the Sim Olympics, where we compete against other residency programs in the area.
Mentorship
Each resident is paired with a career mentor in their desired field, based on their area of interest. This is an opportunity for residents to receive career guidance in their field of interest. Faculty research mentors are also assigned to residents in their PL-1 year. These faculty help residents find project mentors and help develop their ideas into workable original research and quality improvement projects.
Research/Quality Improvement
Each resident is required to participate in a scholarly project during their training. They are free to choose their own topic in an area such as quality improvement (QI)/patient safety, clinical studies, or basic science research. There are ample opportunities for research and our residents are involved in many projects. Residents are also able to take dedicated four-week research electives in their second or third years. Some of the most popular departments for research are PICU, NICU, pulmonology, and hematology/oncology. Additionally, PGY-2 residents spend two weeks on a Quality Improvement/Patient Safety rotation where they work on active QI projects.
Examples of recent resident scholarly project presentations include:
- Impact of an Adolescent and Young Adult (AYA) oncology program
- Effects of implementing a clinical pathway for community-acquired pneumonia
- Incidence of intention to breastfeed among marijuana-using new mothers
- Association of mode of delivery with maternal use of marijuana products
- Effect of sex on glomerular filtration rate in a programmed rat model
- Lifestyle characteristics of parental electronic cigarette users
- Implementation of Clinical Care Pathway Reduces Measles Exposures During Outbreak in New York
- Panel Discussions as an Effective Strategy to Teach Diversity, Equity, and Inclusion in Medical Education
Pediatric Fellowships
Currently, Maria Fareri Children's Hospital offers Accreditation Council for Graduate Medical Education (ACGME)–accredited fellowships in Pediatric Hematology-Oncology, Pediatric Pulmonology, Pediatric Gastroenterology, Pediatric Hospital Medicine, and Neonatal-Perinatal Medicine. Our fellows work directly with residents and provide a great source of education and learning in their specialty.
Resident Initiatives
Buddy Program: A voluntary program to match interns with seniors to help ease the transition into residency
Diversity Committee: The diversity committee organizes resident-led initiatives to bring awareness of, encourage diversity in, and provide a safe space for issues that affect our community. Our group is mentored by the amazing pulmonologist, Marilyn Scharbach. Among other things, we have hosted dinners for new interviewees, started a new mentorship program between NYMC students and residents, and are expanding our diversity education curriculum in coordination with the Assistant Program Director, Dr. Sonia Solomon. We also correspond regularly with the Resident Wellness Committee and the White Coats for Black Lives chapter at Westchester Medical Center. Our learning environment is inclusive and equitable.
The goals of the committee are as follows;
- To promote and celebrate diversity within our program in all respects, including gender, age, culture, race, religion, ability, and sexual orientation, with special attention to groups that are historically underrepresented
- To support learning and working environment that is inclusive to all
- To change perception of marginalized groups in medicine through educational programs
- Partner with NYMC diversity office and provide mentors to underrepresented trainees in pediatrics and those interested in pediatrics
- To provide a venue for discussion and social support surrounding issues pertaining to diversity and inclusion.
Advocacy Day: We pride ourselves in our engagement in group-level advocacy on multiple levels, including local (e.g., our Community Pediatrics and Advocacy rotation), regional (e.g., testifying before local governments in support of children’s health initiatives, and lobbying at our state capital annually), and national (e.g., completing a legislative advocacy rotation with the American Academy of Pediatrics in Washington, DC).
My CHOICE: Started by our residents in 2017, My CHOICE is an elementary school-based program with the goal of educating students on the importance of making good decisions about healthy food. This is a six-week long program where residents go into the classroom (now via Zoom) and teach students the importance of healthy eating and exercise.
Recruitment Committee: A group of residents who want to share their positive residency experiences with applicants through virtual nights-out, resident-led interview sessions, and social media. Speaking of social media, check out our Instagram page @westpedschiefs!
Survival Squad Committee: A group of residents who create a survival guide, full of helpful hints and facts, and brainstorm on other ways to help to make the transition to residency an easier one.
Wellness Committee
At Maria Fareri, we wholeheartedly support efforts to maintain the emotional and mental wellness of our residents. With the introduction of a Wellness Curriculum in 2019 and the development of our resident-run Wellness Committee, we have initiated a program-wide culture shift to recognize and address the challenges associated with being a modern physician. With that, we have dedicated educational time to regular wellness sessions that include didactics and experiential conferences. These introduce residents to concepts of stress management and mindfulness, while practicing talk therapy and meditation. Maria Fareri Children's Hospital's therapy animal program benefits both our patients and our residents, as the gentle animals are available for cuddles for all. We invite you to join us in this exciting new wave of introspection as we learn to be the best version of ourselves as practicing physicians.
Additionally, there is a committee run by pediatric residents that organizes monthly wellness and social events inside and outside the hospital. Residents get together for monthly activities such as hiking, going to the beach, going to the park, getting dinner, and since COVID-19, Zoom get-togethers.
Program Curriculum
Rotation Blocks
The academic year consists of 13 four-week blocks, and the most rotations are four weeks long. Each rotation block consists of a four-week rotation. All inpatient rotations occur at Maria Fareri Children's Hospital. Over the course of three years, pediatric residents are exposed to a variety of pediatric cases, ranging from the typical "bread and butter" to the highly subspecialty-based and complex.
Inpatient Rotation
Each of our three inpatient teams (Rainbows, Ladders and Stars) consist of four or five PGY1 junior residents, two or three PGY2 or PGY3 senior residents, and variable numbers of medical students.
For the two larger teams (Rainbows and Ladders) with five juniors and three seniors, the teams are split into two “hemi-teams” for family-centered rounds. On all teams, PGY1 residents typically have primary responsibility for an average of five patients, although numbers fluctuate by team and time of year. Family-centered rounds are conducted on every team, every day.
- Rainbows (general pediatrics): Our pediatric hospitalists supervise the general pediatrics team, where our residents care for a wide variety of conditions, ranging from common to complex general pediatrics problems. The Rainbows team is split into two teams (Red and Violet) with one senior and two interns on each team.
- Stars (hematology/oncology): Our Stars team is composed of two seniors and four interns and covers the hematology/oncology service, which includes bone marrow and stem cell transplant patients.
- Ladders (subspecialty): Patients admitted to other subspecialty services are cared for by the residents on the Ladders team, our mixed subspecialty team. Our largest subspecialty inpatient services are Pulmonology, Gastroenterology, Endocrinology, Neurology, and Adolescent.
Call Schedule
- After many years as an exclusively 24-hour call program, this year we are transitioning toward a shift schedule on some of the inpatient teams. We are actively seeking feedback from our residents throughout this process, as we work toward the optimal scheduling system for our residents, our patients, and our program. Historically, 24-hour call averages from every fourth to every sixth night. Residents have at least one full weekend off (Friday evening to Monday morning) every block.
- On outpatient rotations, residents cross-cover weekends and weeknights on an inpatient team or in the emergency department three to five times per block. Residents have at least one full weekend off per block.
- In the Emergency Department, residents have a shift schedule. ED rotations are only two weeks long, and shifts are typically ten hours long. There is a PEM attending and senior resident in the ED at all times.
24-Hour Call Example:
Inpatient call schedule example:
7 a.m. - 8 a.m.: Morning sign-out
8 a.m. - 5 p.m.: Regular work day
5 p.m. - 6 p.m.: Evening sign-out from co-residents to assume management of all the patients the resident’s designated inpatient teams.
6 p.m. - 7 a.m.: The overnight team consists of one senior resident (PGY2 or PGY3) and one junior resident (PGY1) on the non-ICU inpatient teams, one senior resident (PGY3) and one junior resident (PGY2) in the PICU, and a fellow and one resident (of any level) in the NICU. After sign-out, the on-call residents continue to manage the inpatient teams, attend to vital patient care, and take on new patients/admissions from the ED throughout the night until sign-out at 7 a.m. the following morning.
Our residents are always supported and never alone, as there is always a hospitalist, intensivist and ED attending in-house 24/7.
Pediatric Emergency Department
Our dedicated pediatric emergency department is a level 1 pediatric trauma center staffed and supervised by board-certified pediatric emergency medicine (PEM) attendings with 24/7 coverage. Our robust emergency department is always busy and provides excellent exposure to a variety of pathology, as well as hands-on exposure to a variety of procedures. The residents work one-on-one with attendings, allowing residents to have high levels of autonomy in our high acuity ED.
Pediatric Intensive Care Unit (PICU)
Rotations in the 18-bed Level I medical/surgical PICU occur in the second and third years. There, residents take primary responsibility for critically ill children with a variety of conditions, including trauma, burns, and post-operative cardiac surgery. There are no PICU fellows, allowing residents to have high levels of autonomy in our high acuity PICU.
Neonatal Intensive Care Unit (NICU)
Residents rotate in our 60-bed Level IV NICU yearly, starting in the first year, where they care for neonates with a wide variety of conditions. The resident team typically consist of two PGY1 residents, one PGY2 resident and one PGY3 resident, who are supervised by a NICU fellow and NICU attending. Residents typically each care for 8-10 patients during their NICU rotation. This academic year, in response to resident feedback, we increased the size of the resident team in the NICU.
Nursery
First year residents spend three weeks in the nursery at Maria Fareri Children's Hospital and one week at a local community hospital nursery taking care of healthy newborns and giving parents anticipatory guidance after the birth of their child.
Elective Rotations
We offer the full complement of core pediatric subspecialty rotations (Cardiology, Pulmonology, GI, Nephrology, ID, etc) all of which are done in house at Maria Fareri Children’s Hospital. In addition, each resident has several blocks in which they have the opportunity to determine their own curricula, including creating their own electives. Past electives have included ultrasound, transport, hospitalist, urgent care, and research.
Continuity Clinic
Residents are allocated one half-day a week at one of nine clinic sites. These sites are located anywhere from five to 30 minutes away from the main hospital campus. Clinic sites range from hospital-based clinics to community-based health centers, to private practices. The wide range of clinics offered allows residents to choose which type of outpatient pediatric clinic they would prefer. Additionally, all residents rotate through our hospital-based clinic. Our residents are also able to transition to a subspecialty clinic site once they have chosen their career path.
Schedule by Year
PL1 Year
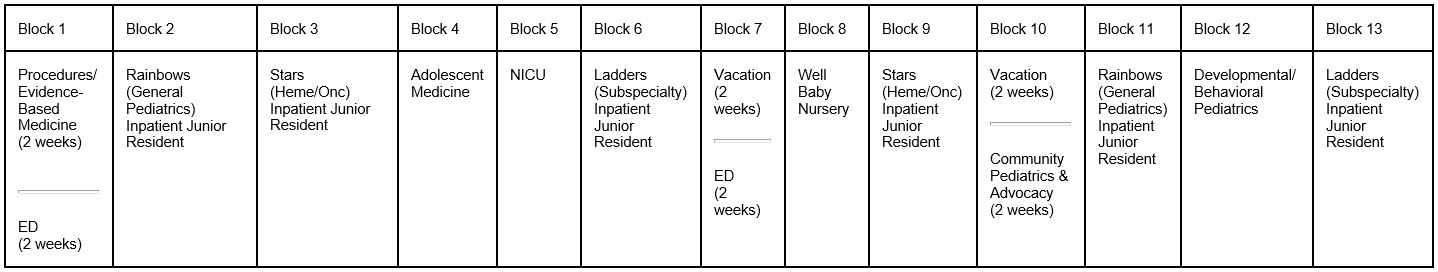
The PL1 resident spends with six blocks on one our three inpatient teams – general pediatrics (Rainbows), mixed subspecialty (Ladders) and (hematology/oncology (Stars) – each in equal measure. The remainder of the year includes one block each of NICU, ED, Well-Baby Nursery, Adolescent Medicine, and Developmental/Behavioral Pediatrics, two weeks of a Community Pediatric Advocacy rotation (CPA), as well as a rotation devoted to improving residents' procedural and evidence-based medicine skills.
During the non-inpatient rotations, the only in-hospital responsibilities are cross-coverage of the ED on weekends, usually two out of the four weeks.
- Inpatient General Pediatrics (Rainbows) Junior: 2 blocks
- Subspecialty (Ladders) Junior: 2 blocks
- Heme/Onc (Stars) Junior: 2 blocks
- ED Junior: 1 block
- Wellbaby Nursery: 1 block
- NICU Junior: 1 block
- Adolescent: 1 block
- Developmental Pediatrics: 1 block
- Community Pediatrics and Advocacy: 1/2 block
- PBLI: 2 weeks
- Vacation: 1 block
PL2 Year
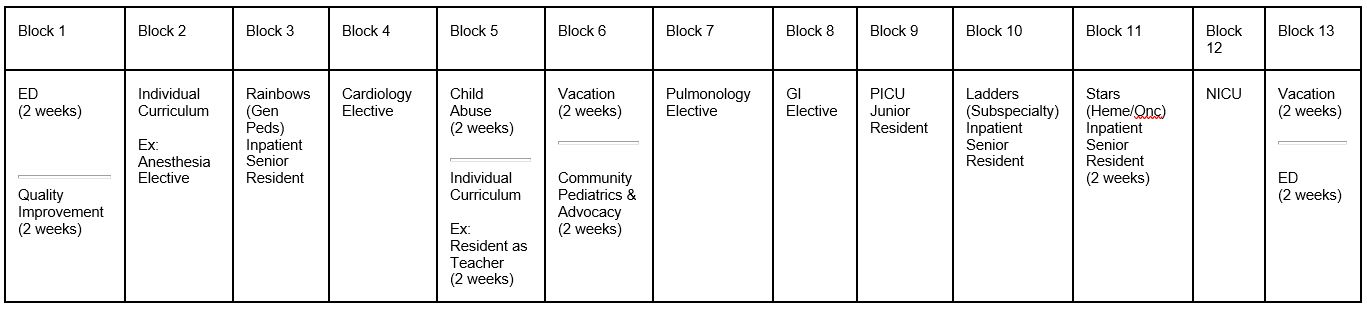
In PL2 year our residents take on supervisory responsibilities for their PL1 colleagues, and also spend time exploring subspecialty interests and other individualized rotations. All PL2s have three months as inpatient senior team leader (split among each of the three teams), plus 2 weeks of Quality Improvement, and one month each of NICU, ED, PICU, Community Pediatrics and Advocacy, and half a month at our on-campus Child Advocacy Center, the regional referral center for evaluation of non-accidental injuries and sexual trauma in children.
The remaining time is spent on subspecialty rotations of the resident's choice (three months), plus one and a half individual blocks, where residents may design their own rotations or choose from among other well-established ones; some popular choices include Research, Resident-as-Teacher, Lactation, and additional supervisory experience in the Well-Baby Nursery.
- Inpatient General Pediatrics (Rainbows) Senior: 1 month
- Subspecialty (Ladders) Senior: 1 month
- Heme/Onc (Stars) Senior: 2 weeks
- ED Senior: 1 month
- PICU Junior: 1 month
- NICU: 1 month
- Elective Rotations: 3 months
- Individualized Rotations: 1.5 months
- Community Pediatrics and Advocacy: 2 weeks
- Quality Improvement: 2 weeks
- Child Advocacy Center (CAC): 2 weeks
- Vacation: 4 weeks
PL3 Year
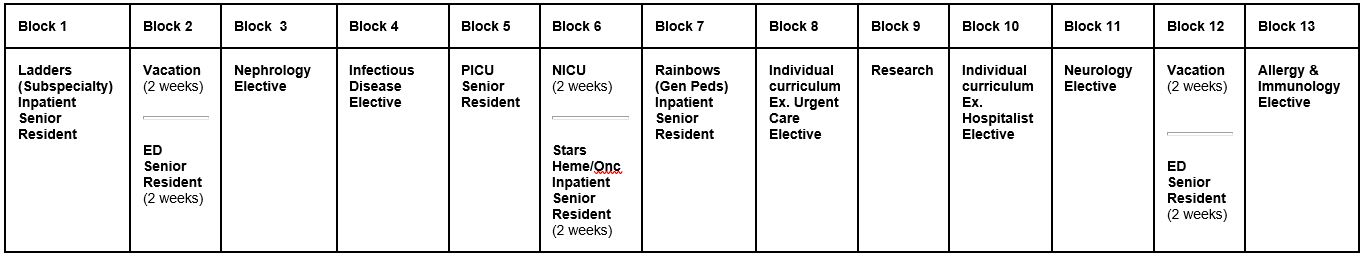
Supervisory responsibilities in the PL3 year include two and a half months as senior resident on the inpatient teams, one month of NICU, one month of ED, and also expand to being senior resident of the pediatric intensive care unit (PICU).
The rest of the year is divided between elective subspecialties and individual rotations.
Most PL3 residents spend their individual rotations preparing for their planned careers: a resident planning a career in outpatient general pediatrics may spend a month at a clinic or private practice, a resident planning a career in emergency medicine may spend a month doing ultrasounds, a resident planning a career as a hospitalist may spend a month as a "pretending" (or "practice attending") hospitalist on the general pediatrics inpatient team, and so on. Residents who feel they need the time may also spend an individual month preparing for their pediatric board certification exam.
Cross-coverage during these rotations is similar to PL2 year, and now also includes PICU coverage.
- Inpatient General Pediatrics (Rainbows) Senior: 1 month
- Subspecialty (Ladders) Senior: 1 month
- Heme/Onc (Stars) Senior: 2 weeks
- ED Senior: 1 month
- PICU Senior: 1 month
- NICU: 1 month
- Elective Rotations: 3 months
- Individualized Rotations: 3 months
- Community Pediatrics and Advocacy: 2 weeks
- Vacation: 4 weeks
Plus
Residents attend their continuity clinic weekly throughout their training. All residents also have one call-free block; most residents use it during their PL3 year – this is a good time to do international rotations or rotations at other institutions if they wish. Many residents in the past have done away rotations at private offices, global health locations, and specialized departments at other hospitals.
General Schedule of Rotations Over Three Years
|
|
|
PL1
|
PL2
|
PL3
|
|
Inpatient Pediatrics
|
General Pediatrics
|
8 weeks
|
4 weeks
(team leader)
|
4 weeks
(team leader)
|
|
|
Hematology/Oncology
|
8 weeks
|
4 weeks
(team leader)
|
2 weeks
(team leader)
|
|
|
Mixed Subspecialty
|
8 weeks
|
4 weeks
|
4 weeks
|
|
|
Well-baby Nursery
|
4 weeks
|
|
|
|
Critical Care
|
PICU
|
|
4 weeks
|
4 weeks
(team leader)
|
|
|
NICU
|
4 weeks
|
4 weeks
|
4 weeks
|
|
Acute Care
|
Emergency Department
|
4 weeks
|
4 weeks
(team leader)
|
4 weeks
(team leader)
|
|
Subspecialty
|
Adolescent Medicine
|
4 weeks
|
|
|
|
|
Developmental Behavioral Pediatrics
|
4 weeks
|
|
|
|
|
Subspecialty Elective
|
|
12 weeks
|
12 weeks
|
|
|
Additional Experiences
|
Community Pediatrics & Advocacy
|
2 weeks
|
2 weeks
|
2 weeks
|
|
|
|
Quality Improvement
|
|
2 weeks
|
2 weeks
|
|
|
|
Individualized Curriculum*
|
|
6 weeks
|
12 weeks
|
|
|
|
Procedures/Evidence-Based Medicine
|
2 weeks
|
|
|
|
| |
Child Abuse Pediatrics |
|
2 weeks |
|
|
|
|
Vacation
|
4 weeks
|
4 weeks
|
4 weeks
|
|
Sample Daily Schedule
|
|
Monday
|
Tuesday
|
Wednesday
|
Thursday
|
Friday
|
|
7 a.m. - 8 a.m.
|
Pre-Round and Sign-Out
|
|
8 a.m. - 9 a.m.
|
Clinical Reasoning Conference
|
Grand Rounds
|
Clinical Reasoning Conference
|
|
9 a.m. - 11:30 a.m.
|
Family-Centered Rounds
|
|
11:30 a.m. - 12 p.m.
|
Patient Care and Clinic Sign-Out
|
|
12 p.m. - 1 p.m.
|
Noontime Core Conference
|
|
1 p.m. - 5 p.m.
|
Patient Care/Afternoon Didactics/Psychosoicial Rounds
|
|
5 p.m.
Sign-out time may vary based on 24-hour vs. shift call
|
Sign-Out to Overnight Residents
|
Fellowship Matches
We are proud of our residents’ success in obtaining competitive fellowship positions in the fields of their choice.
|
2022
|
2021
|
2020
|
2019
|
2018
|
2017
|
|
Allergy/Immunology
Children’s Hospital at Montefiore
Rutgers
Critical Care
MassGeneral Hospital for Children
Penn State
Pediatric Emergency Medicine
Mt. Sinai
Good Samaritan Long Island
Gastroenterology
Children's Hospital of Montefiore (CHAM)
Stony Brook
Maria Fareri/Westchester Medical Center
Heme/Onc
MD Anderson
Children’s Hospital LA
Infectious Disease
NYU Langone
Nephrology
Children’s Hospital of Pennsylvania (CHOP)
|
Critical Care
Cohen Children’s
Cardiology
Nicklaus Children’s
Gastroenterology
Children's Hospital of Montefiore (CHAM)
Hematology/Oncology
Maria Fareri/Westchester Medical Center
Hospitalist
Cohen Children’s
Infectious Disease
Cincinatti Children’s
Neonatal-Perinatal Medicine
Maria Fareri/Westchester Medical Center
Maria Fareri/Westchester Medical Center
Pulmonology
Baylor/Texas Children’s
Nationwide Children’s Hospital
|
Adolescent Medicine
University of Miami
Allergy/Immunology
Downstate
Cardiology
Children's National
Cohen Children's
Hematology/Oncology
MD Anderson
Maria Fareri/Westchester Medical Center
Hospitalist
New York Presbyterian Columbia/Cornell
Infectious Disease
Children's National
Rheumatology
Penn State
Nephrology
Montefiore
|
Allergy/Immunology
Cohen Children’s
Critical Care
Cohen Children’s
Montefiore
Virginia Commonwealth University
Emergency Medicine
University of Connecticut
UT Houston at Texas Medical Center
Global Health
Boston Children's
Neonatal-Perinatal Medicine
University of Florida
Pulmonology
Johns Hopkins
Rheumatology
Montefiore
|
Critical Care
University of Arkansas
Emergency Medicine
Jacobi Medical Center
Oklahoma State University
Endocrinology
New York Presbyterian/Cornell
Infectious Disease
Children's National (2)
Neonatal-Perinatal Medicine
Mount Sinai
Westchester Medical Center
Penn State
|
Child Abuse
Brown
Critical Care
Montefiore
Gastroenterology
Yale
UCLA
Emergency Medicine
Cohen Children’s
Jacobi Medical Center
SUNY Downstate
Hematology/Oncology
DuPont
Cohen Children’s
New York University
Pulmonology
Cincinnati Children's
Nephrology:
Mount Sinai
Neonatal-Perinatal Medicine
Brown
Westchester Medical Center
|
Current Pediatric Residents
Pl-3
Class of 2024 |
Pl-2
Class of 2025 |
Pl-1
Class of 2026 |
|

Jacqueline Benayoun, MD
Medical School: SUNY Downstate Medical Center College of Medicine
Hometown: Queens, NY
Career Goals: To be great to my patients and stay in an academic setting. Potential interests in NICU, endocrine and adolescent health.
Fun Fact: I speak fluent Spanish and I speak/understand a few other different languages!
Accomplishments: Presented at multiple conferences on topics including public health and medical education!
Hobbies: Krav Maga, cooking, puzzles and traveling.
Favorite thing about the program/MFCH: Cool co- interns, the beautiful hospital layout and all the people contained within it!
|

Jessica Adukuzhiyil, DO
Medical School: New York Institute of Technology College of Osteopathic Medicine
Hometown: Putnam Valley, NY
Career Goals:To be a great pediatrician!
Fun Fact:I used to play the flute and the piano
Accomplishments:I am part of the Gold Humanism Honor Society
Hobbies:Hiking, traveling, plants, dancing, cooking
Favorite thing about the program/MFCH: The diverse pathologies that come into the hospital and the welcoming and very supportive environment the program provides.
|

Bhavsimran Anand, MD
Medical School: St. George's University School of Medicine
|
|

Ramon Cabrera, MD, PhD
|

Deepa Badrinath Murthy, MBBS
Medical School:Kempegowda Institute of Medical Sciences
Hometown:Bengaluru, India
Career Goals:A Successful Pediatric Endocrinologist
Fun Fact:Riding the space mountain solo when I was only three years old.
Accomplishments:Trained classical singer
Hobbies:I love to swim, cook during my spare time
Favorite thing about the program/MFCH:Everyone is so warm and friendly and get along really well with each other!
|
Badrinath Murthy, MBBS
Medical School: Kempegowda Institute of Medical Sciences |
|

Haya Chaudhury, DO
Medical School: New York Institute of Technology College of Osteopathic Medicine
Hometown: Huntington, NY
Career Goals: I am considering a career in either Pediatric Emergency Medicine or General Pediatrics!
Fun Fact: I once almost fell off a mountain and to this day, my parents don't know about it.
Accomplishments: I graduated from a seven-year combined BS/DO program
Hobbies: Traveling, Baking, Hiking
Favorite thing about the program/MFCH: My favorite thing about the program has to be the welcoming environment and the family-feel atmosphere.
|

Shreya Bhandari, MD
Medical School: Ponce School of Medicine and Health Sciences
Hometown: Lansdale, PA
Career Goals: Acute care subspecialty (PEM/NICU/PICU), MedEd
Fun Fact: I spend a lot of time on Spotify
Accomplishments: I learned Spanish while studying medicine in Puerto Rico!
Hobbies: Yoga, hiking, trying new restaurants, dancing, making playlists
Favorite thing about the program/MFCH: Everyone in the program is really supportive, cares about your learning, and wants you to become the best pediatrician you can possibly be! Also I love the kid-friendly atmosphere of the hospital.
|

Megan Benn, MD
Medical School: St. George's University School of Medicine
|
|

Madhurima (Maddy) Chowdhury, MD
Medical School: New York Medical College
Hometown: New City, NY
Career Goals: General pediatrics, most likely
Fun Fact: I have a sweet tooth!
Accomplishments: Graduating from medical school in one piece.
Hobbies: Watching TV or tiktok videos, restaurant hopping, reading.
Favorite thing about the program/MFCH: How supportive my co-residents are and how willing everyone is to lend a hand.
|

Simran Bhatti, DO
Medical School:New York Institute of Technology College of Osteopathic Medicine
Hometown: Dix Hills, NY
Career Goals: Not sure yet, but most likely a pediatric subspecialty. Just trying to keep an open mind throughout residency and figure out what I really love!
Fun Fact: English wasn't my first language, Punjabi was! And I have a pet shrimp named Shrimpy!
Accomplishments: Getting published in the JMCC last year and learning how to swim this summer!
Hobbies: Anything food related (cooking, baking, and especially eating), listening to podcasts (my favorite right now is Crime Junkie), bingeing Netflix, traveling and spending time with my family and friends!
Favorite thing about the program/MFCH: The people and the pathologies! Everyone has been so kind and welcoming, it really makes you feel at home and helps foster a supportive environment to learn and grow! Also, there's no such thing as "zebra" diagnoses at MFCH. The hospital caters to such a large scope of patients that you get to see a lot of interesting and sometimes unexpected diagnoses!
|
Brocha Brooks, MD
Medical School: Ruth and Bruce Rappaport Faculty of Medicine, Technion Israel Institute of Technology
|
|

Christopher Ikenna Chukwurah MBBS, MPH
Medical School: University of Nigeria Nsukka
Hometown: Enugu, Nigeria
Career Goals: Pediatric gastroenterology
Hobbies: Playing and watching games like football and basketball. I like to work out.
Favorite thing about the Program/MFCH: It was clear that everyone in the program acted as one family and genuinely cared for each other. The residents were amazing and kind.
|

Keanna Chang, MD
Medical School: University of Connecticut School of Medicine
Hometown: Old Saybrook, CT
Career Goals: Emergency Pediatrics or General Pediatrics
Fun Fact: I taught tree climbing in college, culminating in a trip to the Redwoods in California where we slept at the top of 300-foot-tall giant sequoias.
Accomplishments: I biked across the country from the Washington coast to the Connecticut coast during the summer of 2019.
Hobbies: Rock climbing, running, biking, hiking, eating chocolate
Favorite thing about the program/MFCH: Everyone is always willing to help!
|

James Dalmeny, MBBCh
Medical School: NUI Galway School of Medicine
|
|

Coby Dorfman, MD
Medical School: New York Medical College
Hometown: Toronto, Canada
Career Goals: Undecided
Fun Fact: I am Canadian!
Accomplishments: Raised over $250,000 with my hockey team to help pay for kids cancer treatments!
Hobbies: Running, swimming, playing hockey, and playing with my two sons!!
Favorite thing about the program/MFCH: The residents and the attendings
|

Brianna Cocuzzo, MD
Medical School: Nova Southeastern University College of Allopathic Medicine
Hometown: North Salem, NY
Career Goals: My goal is to be a Neonatologist at a high level NICU with very premature babies. I also want to have a NICU follow-up so I can see the little ones I took care of grow.
Fun Fact: I have two rescue puppies Clare and Kerry. They are real sisters and I have had them since my friend found them outside when they were 6 weeks old. I enjoy taking them for hikes, taking them running, and going to the beach and Starbucks with them.
Accomplishments: Scholarship to medical school for four years based on application and performance. Won an award for best Service Learning Project at my medical school for a Drowning Prevention Project with low income children. Won a President's Choice Award at a Research Conference with my Research Team for a project on the impact of Virtual Reality on Chronic Pain in Children.
Hobbies: Long distance running, I have run marathons in three different countries. Raised money for charities to help children with these events.
Favorite thing about the program/MFCH: Everyone is so nice! Even though it is a hospital with a lot of sick kids, it is not a sad environment. I think we make patients and families feel as much "at home" as possible.
|
Jennifer Gardner, DO
Medical School: Touro College of Osteopathic Medicine
|
|

Irene Fosu-Apraku, MD
Medical School: Meharry Medical College School of Medicine
Hometown: Toronto, Canada
Career Goals: Undecided but interested in hospital medicine or advocacy
Fun Fact: The first part of my last name was given to me in honor of a great uncle
Accomplishments: Watched about 800 episodes of One Piece the summer between first and second year of medical school
Hobbies: Anime, listening to podcasts, reading, soccer, makeup
Favorite thing about the program/MFCH: My co-interns
|

Nydia Correa Rivera, MD
Medical School: Ponce School of Medicine and Health Sciences
Hometown: Lares, Puerto Rico
Career Goals: At the moment I am learning about the beautiful and fascinating world of Children I mean…How Magnificent is that!! I'm intrigued about NICU, Endocrinology and Cardiology! So… Stay tuned.
Fun Fact: I have two furry babies: One dog Duke and one cat called Luna.
Accomplishments: First generation MD and First female member in my family to posses a graduate degree.
Hobbies: Walking outdoors, playing volleyball, watching anime, listening to music.
Favorite thing about the program/MFCH: I get to work everyday with outstanding professionals and human beings. Plus I get to play chess everyday outside.
|
Katherine Gorecki, DO
Medical School: Touro College of Osteopathic Medicine
|
|

Rachel Gecelter, DO
Medical School: New York Institute of Technology College of Osteopathic Medicine
Hometown: Great Neck, NY
Career Goals: Pediatric Subspecialty (GI/Cardio/PICU)
Fun Fact: I was born in South Africa!
Accomplishments: Presenting my first ever podium presentation internationally in Cape Town, South Africa!
Hobbies: Hiking, playing with my dog, traveling, cooking, hanging with friends
Favorite thing about the program/MFCH: The extremely supportive environment and my co-residents!
|

Ghita Elmejjati Burdier, MD
Medical School: Chicago Medical School, Rosalind Franklin University of Medicine & Science
Hometown: Astoria, NY
Career Goals: Undecided
Fun Fact: I have a baby and a fur baby name Eloise
Accomplishments: Fluent in Moroccan Arabic, first person in my family to go to college
Hobbies: Hanging out with my son, Pilates, traveling, trying new restaurants, binge-watching reality tv
Favorite thing about the program/MFCH: The people!
|

Ahmed Haggag, MBChB
Medical School: Tanta University Faculty of Medicine
|
|

Shoshana Howarth, DO
Medical School: New York Institute of Technology College of Osteopathic Medicine
Hometown: Baltimore, MD
Career Goals: To be a Pediatrician who children and families trust
Fun Fact: Mark Andrews is my Favorite Football Player - Go Ravens!
Accomplishments: Recorded over 1,700 miles running, biking, and walking via the Charity Miles app to raise money for the American Diabetes Association
Hobbies: Tennis, hiking, baking
Favorite thing about the program/MFCH: The awesome people I get to work with...and the cool fire truck INSIDE the hospital!
|

Steven (Shloimy) Gold, MD
Medical School: New York Medical College
Hometown: Brooklyn, NY
Career Goals: Something general, still figuring it out.
Fun Fact: I have something like 45 nieces and nephews! I actually lost count!
Accomplishments: Ran three half-marathons together with a friend with Muscular Dystrophy
Hobbies: Sports, reading, family, friends and wine!
Favorite thing about the program/MFCH: The residents! Everyone gets really close, really quickly and is so supportive. I love the people here!
|

May Igawa, MD
Medical School: Sackler School of Medicine
|
|

Bradley Hutton, DO
Medical School: Rowan University School of Osteopathic Medicine
Hometown: Basking Ridge, NJ
Career Goals: Most likely fellowship, NICU or hospitalist
Fun Fact: Before med school I drove across the country with my girlfriend, from Los Angeles back to NJ.
Accomplishments: Was able to DJ in NYC and while abroad in Ireland.
Hobbies: Rock climbing, video games, hiking, audiobooks
Favorite thing about the program/MFCH: All of the jokes and cute things that the kids say even when they are sick in the hospital. Also the fish tanks and the fire truck
|

Kyra Holler, DO
Medical School: Lake Erie College of Osteopathic Medicine, Erie
Hometown: Fort Collins, CO
Career Goals: Probably a fellowship, but I'm not sure what yet! I would also love to be more involved with advocating for my community.
Fun Fact: I became interested in Pediatrics after I had an amazing rotation with attendings who really cared about us as students. This changed the trajectory of my career and has made me really reflect on the way that our mentors shape our futures. Plus, kids are hands-down better than adults!
Accomplishments: Throughout medical school, I became a Licensed Crisis Counselor and volunteered for a local Domestic Violence Shelter. Here, I had the opportunity to directly help victims and their families with safety planning and navigating the legal system.
Hobbies: I love the following: spending quality time with family and friends, reading fiction, yoga, traveling to beautiful new places, shopping, skiing, strong coffee, a well-timed margarita, teaching myself to crochet, trashy reality tv, playing Stardew Valley, avoiding insects at all costs, and spending too much time on Tiktok.
Favorite thing about the program/MFCH: In my short time here, I have been blown away by the support you receive in this program from both the leadership and your peers. A really important aspect of picking a residency program for me was ensuring that I would fit in, feel supported, and be a contributing member of the team. I feel like I will have no problem achieving my goals in this program, as well as aiding others in achieving theirs.
|
Genevieve Ille, MD
Medical School: University of Oklahoma College of Medicine
|
|

Sarah Korn, DO
Medical School: New York Institute of Technology College of Osteopathic Medicine
Hometown: Queens, NY
Career Goals: Pediatric Critical Care/Acute Care
Fun fact: I’m really good at whistling, can whistle almost any tune
Accomplishments: Creating a triage tool for low resource areas. I also ran two half marathons (so practically one whole marathon.)
Hobbies: Biking, puzzles
Favorite thing about the program/MFCH: Friendliness and support of co-residents and faculty. We’re given the space and support to be ourselves and grow in our own way.
|

Scott Lallier, DO
Medical School: Lincoln Memorial University DeBusk College of Osteopathic Medicine
Hometown: Durham, NC
Career Goals: Undecided, maybe cardiology
Fun Fact: Have had three bear encounters in the wild
Hobbies: Frisbee, running, basketball, yoga, meditation.
Favorite thing about the program/MFCH: The people!
|

Heather Jao, DO
Medical School: Burrell College of Osteopathic Medicine
|
|

Jun Young Kwak, DO
Medical School: New York Institute of Technology College of Osteopathic Medicine
Hometown: Queens, NY
Career Goals: Undecided
Fun Fact: I just got my motorcycle license
Accomplishments: Masters degree in nutrition
Hobbies: Playing with my dog, dancing, watching F1, napping
Favorite thing about the program/MFCH: My co-residents and seniors that always look out for one another
|

Aitan Magence, MD
Medical School: New York Medical College
Hometown: Toronto, Canada
Career Goals: I would like to complete a Pediatric Subspecialty, possibly neonatology, pediatric emergency medicine, or child and adolescent psychiatry. I am going into my residency with an open mind! Ultimately, I would like to work in academic medicine as I love teaching and working with medical students to help them achieve their career goals!
Fun Fact: I am Canadian! I am a certified international lifeguard, swimming and canoeing instructor, and have my boating license. I was a university professor, academic advisor, and intern at the NYC Office of the Chief Medical Examiner prior to medical school. I also helped write science content for a number of science-themed board games and helped edit some science-themed children’s books.
Accomplishments: I was inducted as a member of the Gold Humanism Honor Society. Along with an amazing team of educators and advocates, I developed a longitudinal disabilities awareness and inclusion curriculum for healthcare professionals, which has been successfully integrated into the New York Medical College’s School of Medicine curriculum.
Hobbies: Baking, swimming, true crime books and documentaries, writing musical parodies, playing with my nieces and nephews.
Favorite thing about the program/MFCH: The people! I was drawn to pediatrics as a career because of the amazing clinical and ancillary teams that I got to work with at MFCH during my medical school rotations. I loved it so much that I decided to join the MFCH family as a resident!
|
Anna King, MD
Medical School: Louisiana State University School of Medicine in New Orleans
|
|

Sabrina Libretti, DO
Medical School: Lake Erie College of Osteopathic Medicine, Seton Hill
Hometown: Levittown, NY
Career Goals: General Pediatrics
Fun Fact: I won 'Most Distinguished Laugh' and 'Most Likely to Succeed' in my high school's Senior Superlatives
Accomplishments: First person in my family to go to college!
Hobbies: Going to concerts, going to the beach, jigsaw puzzles, and spending time with friends and family
Favorite thing about the program/MFCH: Program leadership who will push you to be the best Pediatrician you can be, state-of-the-art facilities, and a supportive environment created by everyone.
|

Margaret Maloney, MD
Medical School: Stony Brook University School of Medicine
Hometown: Decatur, AL
Career Goals: In-Hospital Care (whether as a hospitalist or otherwise)
Fun Fact: I was a book editor for four years before I changed careers to medicine. When I went back to do my pre-med coursework, the only course requirement I had already filled was in the English Department.
Accomplishments: I have completed internships in both General Surgery and Family Medicine.
Hobbies: I love making things; I quilt and I do needlepoint, and try most crafts at least once. I spend a TON of time hanging out with my grade school age nephews. I'm a fan of all things RuPaul's Drag Race. I read lots of queer romance novels. And I've got a monstera deliciosa plant that's practically a family member at this point.
Favorite thing about the program/MFCH: I rotated at MFCH as a family medicine resident, and fell completely in love with the hospital and the program, and went through the Match again so I could join. My favorite thing is the kids and their families; I love spending time with them on the floor.
|

Mindy Kresch, MD
Medical School: New York Medical College
|
|

Matthew Macoul, DO
Medical School: University of New England College of Osteopathic Medicine
Hometown: New Hampshire
Career Goals: Undecided
Fun Fact: I have the best pit bull in the world
Accomplishments: I cooked meals using just a hot plate for the first month of intern year!
Hobbies: Golf
Favorite thing about the program/MFCH: The people
|

Kimberly Monteferante, MD
Medical School: St. George's University School of Medicine
Hometown: Putnam Valley, NY
Career Goals: Adolescent Medicine Specialist
Fun Fact: I attended the ribbon cutting ceremony for MFCH when I was in first grade.
Accomplishments: I was an All-American collegiate field hockey player.
Hobbies: Crossfit, reading
Favorite thing about the program/MFCH: My co-residents and attendings.
|

Madison Monroe, MD
Medical School: Meharry Medical College School of Medicine
|
|

Macahan Moore, DO
Medical School: Lincoln Memorial University DeBusk College of Osteopathic Medicine
Hometown: East Bernstadt, KY
Career Goals: TBD, but leaning toward General Pediatrics
Fun Fact: I’m really bad at answering surveys.
Accomplishments: I learned how to sail in Greece.
Hobbies: Reading, hiking, board games
Favorite thing about the program/MFCH: The fact that from the moment you enter the hospital the environment is tailored to the children, from the giant aquarium to the full sized train, it provides them with an environment that they can engage with and be provided a distraction from their illness.
|

Patricia Pleta, DO
Medical School: Lake Erie College of Osteopathic Medicine, Erie
Hometown: Oakton, VA
Career Goals: NICU or Adolescent Medicine
Fun Fact: I built my desktop PC
Accomplishments: Black Belt in Gumdo
Hobbies: Video gaming on PC, PS4, and Switch, reading historical fiction novels, watching anime and a variety of movies, and diamond painting
Favorite thing about the program/MFCH: The hospital is beautiful and I love how the residents support each other as we continue to learn.
|

Juliana Nitis, MD
Medical School: Columbia University College of Physicians and Surgeons
|
|

Jai (Ponmali) Photavath, MD
Medical School: George Washington University School of Medicine and Health Sciences
Hometown: Reston, VA
Career Goals: Pediatric Emergency Medicine or Pediatric Hospitalist
Fun Fact: I have two fluffy cats named Clark and Curby!
Accomplishments: I helped implement a clinic-based program linking eligible immigrant families to pro-bono legal services to help increase their access to healthcare services
Hobbies: Rock climbing, painting, museum hopping, trying new food
Favorite thing about the program/MFCH: The incredibly kind, playful, and supportive people!
|

Laura Prunty, DO
Medical School: Touro College of Osteopathic Medicine
Hometown: New York, NY
Career Goals: To be an awesome Pediatrician to many wonderful kiddos- in what subspecialty to be decided!
Fun Fact: I've traveled to seven percent of the world.
Accomplishments: Black Belt in Gumdo
Hobbies: Traveling as seen from my fun facts; finding reality shows to watch on TV
Favorite thing about the program/MFCH: The people! Everyone is so supportive and welcoming. I always feel comfortable asking questions and learning!
|

Sarvani Ramcharran, DO
Medical School: Touro College of Osteopathic Medicine
|
|

Catelyn Rueger, DO
Medical School: Lake Erie College of Osteopathic Medicine, Erie
Hometown: Housatonic, MA
Career Goals: General Pediatrics
Fun Fact: I have met three Olympic swimmers
Accomplishments: I was a member of Sigma Sigma Phi National Osteopathic Honors Society
Hobbies: Swimming and arts and crafts
Favorite thing about the program/MFCH: My favorite thing about the program is the people. Everyone is so kind and welcoming
|

Rochelle Rubinstein, MD
Medical School: New York Medical College
Hometown: Brooklyn, NY
Career Goals: Pediatric Cardiology
Fun Fact: I once donated my hair to make a wig for a child with cancer.
Accomplishments: Best aunt to three cuties. Presented research at a national conference at age 20. American Red Cross Lifeguard Instructor. Learned how to scuba dive in Israel. I taught myself how to solve a Rubik’s cube.
Hobbies: Hiking, Biking, Painting, Swimming.
Favorite thing about the program/MFCH: The people who really work hard to create such a warm and supportive program and child and family friendly hospital. Also the sculptures on the front lawn.
|

Puneet Singh, DO
Medical School: New York Institute of Technology College of Osteopathic Medicine
|
|

Lauren Santos, MD
Medical School: St. George's University School of Medicine
Hometown: Dartmouth, MA
Fun Fact: I'm in the process of teaching myself the latest pop hits on my niece's Fisher Price Xylophone. Also, my sister and I were once in a Disney World parade!
Accomplishments: I was peer-nominated and inducted into my medical school's chapter of the Gold Humanism Honor Society.
Hobbies: I love all things Disney, the Hamilton soundtrack, a good Target run, and asking to pet every dog I meet. Spending time with my niece while doing all of the above is just the icing on the cake.
Career Goals: I'm still exploring the world of Pediatrics - current interests are hospitalist and NICU! Ultimately, I hope to grow lasting, meaningful relationships with my patients and their families. I also want to get involved with medical student education to inspire future Pediatricians!
Favorite thing about the program/MFCH: MFCH was my very last interview of the virtual season. Hands down, it was the interview day where I smiled the most and felt the most "at home." From the beautiful facilities, child-friendly design, and resident camaraderie to opportunities for advocacy and community outreach with a diverse patient population - I'm so happy to be a part of the MFCH family with my great co-residents!
|

Srujana Sattari, MBBS
Medical School: Kamineni Institute of Medical Sciences
Hometown: Grafton, MA & Hyderabad, India
Career Goals: Plan on doing a fellowship, not sure which one yet.
Fun Fact: I've lived half my life in the US and the other half in India.
Accomplishments: I'm a black belt in karate.
Hobbies: All things mystery! Books, movies, TV shows. Enjoy being active and on my feet, whether it's on a hike or a stroll or playing a sport.
Favorite thing about the program/MFCH: It's a great group of people, very welcoming and supportive. Love that the hospital is very oriented towards kids, including the fire truck, the fish tank, and the baseball hall!
|

Victoria Siracusa, DO
Medical School: Touro College of Osteopathic Medicine
|
|

Eliana Segal, MD
Medical School: Rutgers New Jersey Medical School
Hometown: Teaneck, NJ
Fun Fact: I drove my first car from Texas to New Jersey with just a learner's permit
Accomplishments: Cooking dinner almost every night even with a busy resident schedule! Also, planning my wedding while successfully completing my first year of medical school.
Hobbies: Baking, reading, painting, hanging out with friends and family, Netflix
Career Goals: Pediatric subspecialty (Emergency Medicine, PICU)
Favorite thing about the program/MFCH: How supportive everyone is! The seniors are always there to guide and assist, the interns help each other chug through the long days of work, and the faculty and administration go above and beyond to integrate our personal lives into our busy schedules.
|

Rouba Sayegh, MD
Medical School: Lebanese University Faculty of Medical Sciences
Hometown: Beirut, Lebanon
Career Goals: Pediatric infectious disease
Fun Fact: I love cakes, if you see me with cake, please take it away from me!
Hobbies: Hanging out with family and friends, baking, reading, hiking.
Favorite thing about the program/MFCH: Very friendly atmosphere, the giant chess set
|
Adira Teitelbaum, MD
Medical School: SUNY Downstate Medical Center College of Medicine
|
|

Christine Vu, DO
Medical School: A.T. Still University School of Osteopathic Medicine in Arizona (SOMA)
Hometown: San Jose, CA
Fun Fact: The first thing I do whenever I move to a new place is look up the closest boba store and the surrounding food scene.
Accomplishments: I was part of a project in medical school where a group of us provided weekly health education presentations to refugees in our community. Our project was presented at the 2021 National Association of Community Health Centers Expo.
Hobbies: Going on food adventures, exploring new cultures, traveling, being a plant mama, and lots of crafting.
Career Goals: Undecided, going into residency with an open mind!
Favorite thing about the Program/MFCH: The people - our program director, co-residents, attendings/preceptors, administrative staff, and hospital staff to name a few. Everyone here is so supportive of one another and sincerely cares about your well-being and career goals.
|

Elisa Schunkert, MD
Medical School: Universität Witten/Herdecke Fakultät für Gesundheit
Hometown: Boston, MA and Munich, Germany
Career Goals: To become a competent & compassionate physician, with an interest in research and teaching.
Fun Fact: I saw the peak of Mount Everest!
Accomplishments: Graduated a three-year post-doc research fellowship in dermatology on GvHD and severe drug reactions at the Brigham & Women's Hospital, HMS.
Hobbies: Running, hiking, traveling, spending time with my husband and daughter
Favorite thing about the program/MFCH: Excellent faculty and fabulous, supportive co-residents.
|

Ruba Abdul Wahed, MD
|
|
|

Joseph (Yosef) Schwob, DO
Medical School: New York Institute of Technology College of Osteopathic Medicine
Hometown: Baltimore, MD
Career Goals: Undecided
Fun Fact: I had a new baby, two weeks after Match Day
Accomplishments: I ran two half marathons, both in under two hours!
Hobbies: Spending time with family, running, listening to music.
Favorite thing about the program/MFCH: Supportive faculty and vibrant camaraderie amongst the residents.
|
Angela Wang-Negri, MD
Medical School: New York Medical College
|
| |

Joel Thomas, MD
Medical School: SUNY Downstate Medical Center College of Medicine
Hometown: Syosset, NY
Career Goals: Still deciding! Looking for something challenging and pathophysiology focused.
Fun Fact: Crocodiles cannot stick their tongue out. Oh, you meant my fun fact? I am a big fan of Marvel/DC superheroes! My favorite is, obviously, Spiderman.
Accomplishments: I have been working with kids through organizations/non-profits since middle school!
Hobbies: Non-profit work, camping, going down rabbit holes, and reading history (I will easily spend all day in a museum).
Favorite thing about the program/MFCH: The people and the autonomy residents have! Plus, the hospital is clearly designed for kids.
|

James Worfolk, MD
Medical School: Eastern Virginia Medical School of the Medical College of Hampton Roads
|
| |

Lila Yang, DO
Medical School: New York Institute of Technology College of Osteopathic Medicine
Hometown: Scarsdale, NY
Career Goals: NICU
Fun Fact: My favorite breakfast dish is a fried egg with sriracha and peanut butter on toast! Sounds odd but it’s really yummy!
Accomplishments: I have been working with kids through organizations/non-profits since middle school!
Hobbies: Hiking, traveling, biking, trying new cafes and restaurants, yoga, and learning to cook!
Favorite thing about the program/MFCH: The incredibly friendly and supportive co-residents and faculty!
|
Michael Young, DO
Medical School: Philadelphia College of Osteopathic Medicine
|
| |
|
Past Pediatric Residents
Class of 2023
Yaritzy Michelle Astudillo, MD
Kristina Bezdickova, DO
Dan Brady, DO
Maria Cabrera-Hernandez, MD
Victoria (Tori) Close, MD
Max Cohen, DO
Charne Delport, DO
Elissa Dunlap, DO
Svetlana Duvidovich, DO
Aliza Grabie, MD
Brian Gu, MD
Marilyn Huamantla, MD
Chantel Johnson, MD
Ariella Kashi, MD
Yevgeniy Liverant, MD
Wenona Lok, DO
Angelo Louvros, DO
Alexis Mandon, MB, BCh, BAO
Alexandra (Sasha) Mazo, MD, PhD
Dave Plaza, MD
Menachem Rimler, MD
Class of 2022
Paul Mandaro, MD
Deena Miller, MD
Moshe Apfel, MD
Taya Carpenter, DO
Elysia Cohen, MD
Rachel Finkel, MD
Rachel Friedmann, DO
Aaron Grubner, MD
Josh Hanau, MD
Dana Convissar Kessler, DO
Sepeedeh Kermalli, DO
Nevine Macalintal, MD
Shanel Mehta, DO
Samantha Pravder, DO
Roma Shah, DO
Olivia Shyong, DO
Keila Sole, DO
Daniel Steiner, MD
Heidy Wang, MD
Rebecca Wachter, MD
Class of 2021
Olubusayo Mercy Akinyemi, MD
Najveen Alvi, MD
Junhong Ao, DO
Clare Bozso, DO
Kayleigh Clark, MD
Stefanie Kagan, DO
Sonam Kapoor, DO
Jennifer Kaswick, MD
Nasim Khattab, MD
Julia Kim, DO
Blake LeGrand, MD
Amy Lu, MD
Paul Mandaro, MD
Deena Miller, MD
Catherine Murphy, MD
Melani Olivares, MD
Kelly Parness, DO
Rachel Ronau, DO
Nehal Shah, DO
Chantal Talmor, MD
Kristen Wallace, DO
Resident Life
Our program prides itself on establishing close bonds among co-residents from day one. From the beginning at orientation to the final days at the graduation dinner, we truly become a family.
MFCH is located in Westchester County, New York. We are in the historic Hudson Valley region, a suburban area about 25 miles north of midtown Manhattan, and surrounded by the gorgeous Hudson River and Long Island Sound.
New York City is directly south of Westchester County, and Grand Central Station can be reached from MFCH by a 30-minute drive or a 25-minute train ride. NYC offers everything: a picnic in Central Park, cityscapes on the "Top-of-the Rock" at Rockefeller Center, Broadway shows, the Bronx Zoo, professional sports (the Yankees, the Knicks, the Rangers, the Giants, and the Jets), concerts, and some of the best and most diverse restaurants in the world.
Quick access to New York City is only one of the benefits of living in Westchester County. MFCH is a quick, 5-minute drive away from White Plains, which is the commercial and cultural hub of Westchester County. It offers an active nightlife, fine dining, performance arts, great living accommodations, and many shopping centers. It is the most popular place to live among our residents, although many of our residents also live in and commute from NYC.
The Hudson Valley region offers enormous opportunities for outdoor activity of all types: hiking, cycling, climbing, and just relaxing. One highlight is Bear Mountain State Park, a 40-minute drive north of MFCH. Located on the west bank of the Hudson River, this park offers hiking, biking and cross-country skiing along the Appalachian Trail, shaded picnic and camping areas, and opportunities for lake and river fishing. There are many beaches lining the Hudson River, Long Island Sound, and Atlantic Ocean, all within easy driving distance from MFCH.
Westchester has everything you'll need for creating a wonderful living experience.

Maria Fareri Children’s Hospital

Halloween Fun; Disney Heroes vs Villains

Thanksgiving Potluck

Birthday Celebrations

Baby Shower Celebrations

Class of 2021 at their Intern Outing!

Class of 2022 at their (masked but not particularly socially-distanced) Intern Retreat!

Our monthly End of Block Rotation Parties!

Advocating for children at AAP Advocacy Day in Albany
View more photos capturing resident life
How to Apply
Our residency program participates in the National Resident Matching Program (NRMP) through the Electronic Residency Application Service (ERAS). Applications are only accepted through ERAS. Applicants may apply to three-year categorical pediatric positions, as well as one-year and two-year pediatric preliminary positions.
Our ACGME Identification Number is: 3203511176.
Application Requirements
Through ERAS, please submit the following:
-
Personal statement
- Curriculum Vitae
- Photograph (optional)
- Medical School transcript
- Medical Student Performance Evaluation (MSPE) Letter
- Three Letters of Recommendation
- USMLE scores
- If applicable, your standard certificate from the ECFMG. This is required prior to the start of residency.
Match Timeline
ERAS Opening Day: September 6, 2023
Applicant Interviews: Tuesdays and Thursdays, October to February
Match Day: March 15, 2024
Pediatric Orientation: June 24-28, 2023
Pediatric Residency Start Date: July 1, 2024
Criteria for Selection to Interview
We take a holistic approach to application review and have no specific cutoffs. We accept both USMLE and COMLEX scores. Please note: we do not have any cut off scores for USMLE or COMLEX tests. There is also no cut off for year of graduation from medical school. We review all applicants from a holistic standpoint, taking into account their overall diversity, skills, and experience. We also sponsor J-1 visas.
Interviews
All applications received prior to November 15 will receive equal consideration. Interview invitations will be offered throughout the season on a rolling basis on Tuesdays and Thursdays, October through February, and interview invitations will be sent throughout the season as new slots open up. Interviews for invited applicants will be offered via Zoom, the video conferencing platform. During the interview, applicants will be able to watch and participate in clinical reasoning conference, learn about the program from the director, interview with faculty, virtually tour the hospital, and chat with residents during (virtual) lunch.
Meet-and-Greets
This year, these get-togethers will occur virtually over Zoom. Applicants invited to interview will receive a schedule of these events; an interactive activity is planned for each.
Contact Us
For More Information About Our Program…
Ms. Woolf (Coordinator) - beth_woolf@nymc.edu
Dr. Kapklein (Director) - Matthew_Kapklein@nymc.edu
Dr. Chantel Johnson and Dr. Alexis Mandon (Chief Residents): WestPeds@wmchealth.org
914.493.6669 or 914.493.6447